3 Health Myths - Antidepressants and tranquilizers
We've already talked about all three here, albeit “lightly”, but I thought it would be good to delve a little deeper... Not least because patients in my practice rarely have any doubts or misconceptions about at least one of these subjects (most of them about all of them).
MYTH: “The main treatment for depression/anxiety is antidepressants/anxiolytics”
Honestly, do you know anyone who has been cured of anxiety, depression or panic disorder (from now on I'll call it ADTP, to make it easier - although it's not an official nomenclature) as a result of treatment with antidepressants or anxiolytics (also called “tranquilizers”)? I don't. That's because most antidepressants/calming drugs don't act on the causes of ADTP, but rather by making the neurotransmitters stay longer in the synaptic cleft or by acting directly on the receptors (respectively), and not by increasing their production or optimizing their release into the cleft... Is that complicated? Then let me explain it simply:
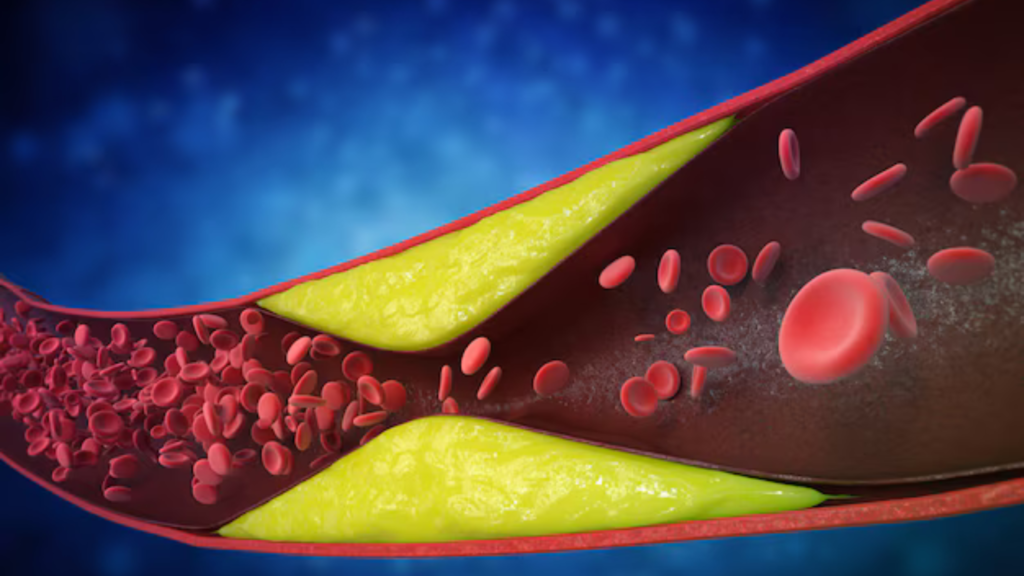
Nerve stimuli are conducted by nerves, which are bundles of neurons (nerve cells) working together in sequence to conduct specific electrical impulses (nerve stimuli, which can be pain, tactile sensations, emotions, etc.). In other words, every sensation or emotion, in order to be felt, needs to be transmitted from one neuron to another, successively. It so happens that one neuron never touches another (or this would cause a “short circuit”), which means that when a message needs to be transmitted from one to another, a “bridge” needs to be created between them; this bridge is the neurotransmitter: it is released into this communication space (synapse) between the neurons (the synaptic cleft), allows the stimulus to pass through and is then removed from there (by reuptake or destruction).
Our brain has many different neurotransmitters: Dopamine, GABA, noradrenaline, acetylcholine... But the main one, when it comes to satisfaction and pleasure, is serotonin; so much so that serotonin is involved, alone or together with other neurotransmitters, in more than 80% of ADTP cases. The fact is that reductions in the amount of serotonin available in the synaptic clefts (a lack is the most common disorder, excesses are rare) lead to anxiety, depression, panic or combinations of these, with severity, periodicity and characteristics depending on this amount.
So, if the problem is the amount of serotonin available, the key to ADTP treatment should generally be to increase it, right? Or perhaps include other neurotransmitters? It's not that simple:
✅ Causes: Either you treat them or the patient will spend a lifetime relying on medication to feel better. Most antidepressants and tranquilizers don't act on the causes of ADTP, remember? This is because the factor that leads to the reduction in available serotonin is still present. Stress and poor diet, along with hormonal disturbances and individual genetic tendencies towards ADTP, for example, are the most important factors that reduce serotonin. Poor diet reduces the bioavailability of precursors needed to make serotonin - yes, the raw material for making everything in the body comes from proper nutrition! - and stress, because it chronically consumes both the raw material for making neurotransmitters, for example, vitamin B6 and magnesium, and the neurotransmitters themselves, while at the same time disrupting hormonal balance. And hormonal disturbances are indisputably important factors in causing, maintaining and worsening ADTP.
✅ Production: There are five basic ingredients needed for the brain to produce serotonin: tryptophan (an amino acid), vitamin B6, folic acid and magnesium, in the presence of a little carbohydrate. A lack of any of these elements prevents the brain from synthesizing serotonin. It turns out that most of the world's population lacks these nutrients in their diet, especially the B vitamins and magnesium. What's more, stress - perhaps one of humanity's most common disorders - also competes for these same nutrients.
✅ Recapture: As already mentioned, one of the most common strategies used by drugs is to reduce or inhibit the reuptake of neurotransmitters in the synaptic cleft, with the belief that this would leave more of them available to act and for longer. The point is that the neurotransmitter is designed to be released, to act and to be removed, right? This is because, when it stays in the cleft for too long, it can also lead to forms of ADTP (for example, depressed patients who, with the use of the drug, become increasingly anxious).
✅ Direct action: Several drugs, especially benzodiazepines, known as “tranquilizers”, act directly on receptors, mainly the neurotransmitter GABA, either by stimulating or blocking them. In this case, another problem arises: how to properly control the degree of this direct effect and deal with the need for ever higher doses to achieve it?
But how many conventional treatments for ADTP do you know that address these basic issues? I may be wrong, but what I see most often is medication being prescribed too early, while the recommendation in the literature is clear: it should be an adjunct to treating the causes, and not something “perpetual”. In other words, reducing stress, having good psychological support and a proper diet, or even associated with good supplementation, are more likely to treat successfully and without causing ADTP dependencies than the isolated use of medication. Only those who don't want to can't see it.
In summary, not only for PTAD but for any disorder, addressing the signs and symptoms with a view to relieving the patient is noble and often necessary. But if their cause isn't treated at the same time, the patient won't get a cure or sustained and progressive improvement, becoming increasingly dependent on medication to feel well. And let's face it: what kind of medicine is it that turns sufferers of organic imbalances, sometimes transient and/or self-limiting, into drug addicts?